Founder resources for weathering COVID-19
For the foreseeable future, Bessemer will answer pressing questions founders have amidst the Coronavirus pandemic and its impact on startups and the entrepreneurial ecosystem.
There's no doubt that COVID-19 has been highly disruptive to society, business, and what we considered to be "normal life" up until now. From transitioning to remote work policies in a hurry, assessing risk and strategic planning under these new economic circumstances, and managing teams through a crisis, we're seeing how founders are grappling with the COVID-19 pandemic. These challenges require entrepreneurs to grow into the leaders they've always aspired to become, and the Partners at Bessemer are here to provide counsel as we all navigate this global health crisis and subsequent shifts in the economy.
On behalf of our Partners, we're curating quick-guides for founders as they weather these uncertain times. Every week, Bessemer will share updates, insights, and best practices on topics to help first-time founders stay-up-to-date on the questions that might be keeping them up at night. But don't lose hope—we also highlight the helpers and silver linings founders can take as the fuel and inspiration.
Questions:
- What are the experts saying about COVID-19?
- What are the opportunities for founders given the COVID crisis?
- How should I think about cash management and fundraising in an economic downturn?
- How should I value my startup during a downturn?
- How can I manage churn and customer retention rates?
- What are the metrics that matter most right now for enterprise software companies?
- What are the best practices to transition to work from home (WFH) in a hurry?
- What are the ways that I can contribute to the cause?
- What good news can I read?
Read the insights and answers to these questions below. To get updates sent to you on a weekly basis, subscribe to our newsletter. If you are a founder navigating challenges and you have a question for our partners, reach directly out to us on Twitter at @BessemerVP or LinkedIn.
Q: What are the experts saying about COVID-19?
On A Healthy Dose, Partner Steve Kraus and his co-host and friend Trevor Price of Oxeon Partners interview experts, leaders, and practitioners on the state of the healthcare industry. In this special mini-series, they speak with the experts on the pandemic outbreak.
CEO Donny Tuchman of Cobble Hill LifeCare on caring for elder populations in pandemic hotspots

In the tenth episode of A Healthy Dose COVID Crisis miniseries, Trevor and Steve talk with Donny Tuchman, CEO of Cobble Hill LifeCare. Donny talks about how Cobble Hill's frontline workers are managing care for its nursing home residents in Brooklyn, a hotspot of the pandemic.
Key takeaways from this episode include:
- Fresh perspectives on what care optimization means at a skilled nursing home facility: “Optimization is about meeting the needs of the resident where they are and trying to help them along with their families. Imagine, what is the optimal quality of life that this resident, this person, can achieve wherever they are? If it's a short term rehab patient, it’s—’How can we as quickly as possible get you back on your feet and get you back home? And how can we help you transition back home without bouncing back to the hospital?’ To a long term resident who has their own unique situation and needs, to the palliative care resident, it's about, ‘How can we help you live out your days? How can we help you have a peaceful, comfortable end?’"
- The challenges of COVID-19 preparedness for the elder population: “In the second week of April, I know we had 50 concerning cases already, where we suspected. Fairly early on, the Department of Health actually came out with guidance saying that we actually shouldn't be testing, and we don't need to test. If we reside in a community where there's widespread community transmission, to just assume that based on symptoms only, the residents have it. And then to just put these practices in place, infection control, do the best we can under the circumstances. So it was pretty quick...we calculated at one point that we probably would need around six to 8,000 gowns, for example, a day, a day, to just manage our population. (When we're full, we're at 364 beds and we typically run 90, 98% occupied.) During this process we made a deliberate decision to bring our census down, particularly because the staffing was just, it was really, really dire. At the height of this, we lost a third of our staff that were out sick.”
- Managing grief and the emotional toll COVID-19 has had on nursing staff: “So when our residents are dying for whatever reasons, and especially when they're dying in large numbers and in a very concentrated period of time, that's very, very traumatic for the staff. So we were grieving with them....We have all fought valiantly to protect our residents, to be transparent with our family members and to do the utmost that we could to honor and respect them. But as a leader, my objective was equally to my team, to support them as well as to our residents and to their families.”
- The future of skilled nursing facilities: "When I assumed CRO, a couple of years ago here, it was really about parallel paths. One: How could we create a highly effective skilled nursing facility to optimize care? Two: How do we recruit a team of people who were innovators and entrepreneurs to be able to imagine and to envision what are the needs going to be in 20 years from now? How do we think about how to bring the services to our residents? What kind of services will they need? How do we leverage technology? We are a traditionally resource poor industry. Everything comes to us last and you know, my personal belief is that if it's typically built for the skilled nursing facility, it's probably pretty mediocre. So we have to start to think much more broadly, much bigger, develop moonshot ideas of how do we really innovate and optimize? And stop thinking in this really small minded way about what's here, right in front of this right now, and just putting out fires and responding to the crisis of today.”
David Shulkin, M.D. on serving veterans and the role of government in a public health crisis

In the ninth episode of the A Healthy Dose COVID Crisis miniseries, Trevor and Steve talk with David Shulkin, the ninth Secretary of the U.S. Department of Veterans Affairs who served under President Donald Trump. He was the Under Secretary of Veterans Affairs for Health from 2015 until 2017, appointed by President Barack Obama. Before his work in government, David also led as Chief Medical Officer at UPenn and ran a value-based organization at Atlantic Health Care.
Key takeaways include:
- How value-based care vs. fee-for-service systems compare during COVID-19: “This crisis has really amplified and exposed all the different dysfunctions of a healthcare system and has exacerbated those that were more fragmented and allowed those that were more integrated and consolidated to function even better because this requires people to communicate,” prefaces David. “It requires people to share data, share resources, think together, and so some of those organizations, those value-based organizations that you've talked about, are just further along in terms of being an integrated model; that means that their communication and their ability to work together and break down the silos is already more advanced than some of those that were in the more traditional model. However, it's really not a reimbursement or a business model issue here. It's really more the extent that the organization works together and people work together.”
- Whether the COVID-19 outbreak in the U.S. is a failure of our public health system or a failure of communication at the federal level: “I believe people in public health and in academics are going to be asking for the next decade as they look back upon this crisis. For me, this really highlights what the role of government is. And over the past couple years we have gotten so used to government being about partisanship and political games and people got so turned off to it, and now we recognize the real role of government is to protect the safety of its citizens,” said David. “Now that we are in a pandemic and a public health crisis, we recognize that this is the role of government—to be looking out for surveillance, to be looking at how we respond when there is a public health issue, to be coordinating these resources, to be providing things for citizens that local governments can't do. Frankly this has exposed us to the fact that we’ll have to reinvent the way that the governments at the federal state and local levels work with the private sector in order to be able to fulfill the real role and function of what the government should be doing.”
- The massive scale of The Department of Veteran Affairs: “The VA is the largest healthcare system in the country and it's the second largest government agency. So first you have the Department of Defense and then you have the Department of Veteran Affairs,” explained David. “The Department of Veteran Affairs has over 400,000 people in it. To give you a comparison, the Department of State has 20,000 people in it. And so the budget of VA is now around $220 billion, although they just got another $19 billion in the first Cares Act. So it continues to have extensive resources. It has more doctors, nurses, pharmacists, psychologists, social workers employed than any other health system, and about 1100 facilities across the country and serves veterans across the world wherever they live.”
- Why veterans are an at-risk population for COVID-19: “There's about 20 million American veterans, about half of them, just under 10 million, get their care at the Department of Veteran Affairs healthcare that is,” said David. “The Veteran Affairs Department serves largely as a safety net population—those people that were injured during their service or meet certain economic levels where they are unable to afford healthcare in other environments. So it's a place that many people rely upon to get their healthcare. Many veterans live in rural parts of the country where healthcare resources are scarce and you can't find specialists and certain healthcare professionals. The average age of our Vietnam veterans, our largest group of veterans, is now above 70 years old, so those that do need care tend to be older and sicker, with about 60% having a comorbid diagnosis in a behavioral health category.”
- The importance of telehealth for veterans during the pandemic: “The number one issue that I established as the top clinical priority when I was Secretary and remains the priority at VA today is suicide prevention. Twenty veterans take their life every day,” said David. “That is a much higher proportion than you would find in the general population, and so when you isolate people and you add stress and the economic impact of this pandemic on people, there is certainly going to be very severe consequences here,” he continued. “So you have to battle that in ways that I think are effective. The most effective way to do that, particularly in the veteran population, is peer support and people reaching out who understand what the veteran experience has been. That's something that VA has learned and does well, and telemental health and organizations are critical for veterans at this time.”
Governor of Rhode Island, Gina Raimondo on managing public health and economic security during COVID-19

In the eighth episode of the A Healthy Dose COVID Crisis miniseries, Trevor and Steve talk with Governor Gina Raimondo, the Governor of Rhode Island. “This coronavirus has massively and significantly accelerated many of the trends that were happening in our economy. Public sector leaders have a serious obligation, as do private sector leaders, to help support the businesses and people most impacted,” Governor Raimondo said. “Corona has devastated people and businesses and I believe we have an obligation to train them up and give them a chance to compete.”
Key takeaways from this conversation include:
- The role of the federal government during this global pandemic: “When you're fighting a global pandemic, a global public health crisis, it's appropriate for the federal government to lead. Every state should be led by them, and then of course every governor has to respond to the conditions on the ground,” she explained. “The whole reason we're in this mess is because at a federal level, we have disinvested in public health infrastructure for a long time. And so when the crap hits the fan as it is now with this virus, the national stockpile was not even close to what it needed to be. We all opened the cupboard for the national stockpile and there wasn't enough there,” Governor Raimondo continued. “This craziness of telling states to each go into the private market to buy what we need, and oh, by the way, compete with the federal government, that is not how it's supposed to work. If we had a robust public health infrastructure federally, which is what we should have, we would be in a whole much better place. By the way, within that, every governor still could do what they needed to do. We could invest more in certain places; for example, my state looks different than every other state. It's very densely populated. We have a high immigrant population, obviously I have to do different things than Idaho, Wyoming and Montana. But the fact of the matter is the federal government just isn't doing, didn't do, wasn't ready to do what it should have done.”
- The vital importance of building a public health infrastructure at the state level: “I'm very proud of the fact that in Rhode Island, we have a 3% uninsured rate. Ninety-six percent or more of Rhode Islanders have health coverage and that's a great thing. Going into a pandemic of this kind, the last thing people need to stress out about is, can I go see my doctor, can I get a test, can I go to the ER, can I go to the hospital? And so while our system is far from perfect, it's pretty good. It's better. We have almost no children who are uninsured and that's a good thing. Also though, I have moved quickly to build many public-private partnerships,” said the Governor. “Like any CEO, you've got to get the job done. I had to get the job done. So if the federal government wasn't going to deliver tests, I had to reach out to other areas. So for example, we reached out to CVS, which is headquartered in Rhode Island, and they saved the day. We worked with them, they partnered with us, and with Abbott. I brought the national guard to provide manpower, and we tested over a thousand people a day at the one CVS drive through testing site.”
- The delicate balance of managing economic insecurity and public health risks: “There's no question that there's a relationship between economic health and physical health. Being out of work for a long time is going to make people less healthy, mentally, and physically. That really weighs on me,” said Governor Raimondo. “You know Steve, I have spent six years blindly focused on getting Rhode Island's economy back. When I was elected governor, Rhode Island had the highest unemployment rate in the country. And I got elected and widely reelected because I talked all about creating jobs, and before this happened, our economy was rocking and rolling, so it killed me to shut down businesses. I want to be pretty aggressive, on the safe side of aggressive, around bringing back businesses. So for example, I never shut down manufacturing. That was a difference between Massachusetts and me. So far, that's turned out to be a good decision.”
Kevin Tabb, M.D., on the Boston area’s innovative and collaborative response to COVID-19
In the seventh episode of the A Healthy Dose COVID Crisis miniseries, Trevor and Steve speak with Kevin Tabb, President and CEO at Beth Israel Lahey Health, and is one of the most prominent and respected health system leaders in our country. In this conversation, they discuss the challenges of running a hospital in these harrowing times.
In this conversation, they discuss:
- How COVID-19 is disportionally impacting communities of color: “In terms of payer-mix at Beth Israel Lahey Health in Boston, we're roughly 50% commercial and 50% governmental, made up of mainly Medicare, but also a significant portion of Medicaid. But what we're seeing that is really very, very disturbing is that more than 40% of the COVID-positive patients in our ICUs that are intubated come from a very small number of neighborhoods, towns and 30 to 40% of the patients are from Latinx and black communities,” said Kevin. “That is very, very different than what we historically see. Often they would make up somewhere between 15 and 17% of our historical discharges. If you walk into our ICUs, you are struck by how much this has hit, disproportionately, a number of communities of color.”
- Why the United State’s response has lagged compared to other countries: “There are some countries that were able to mobilize really quickly in ways that were very effective. Singapore certainly comes to mind, but you don't see the scale that you see in this country or in China or in Europe. The challenges here have to do with that this is unprecedented, first of all, there's nobody that believed or imagined that it would get as bad as it is,” said Kevin. “I think many people knew and believed that a pandemic was coming. There's no question. But I think there was not a prediction that this one would end being as devastating as it was, combined with global supply chain issues. So we're dependent on a global supply chain that has shut down in a global pandemic, and it's really a wreaked havoc. We'll probably change the way that we think about how we procure and how we rely on ourselves on stuff produced in this country. I think that there's a lot of soul searching going on at the moment.”
- How hospitals are collaborating in the Boston area: “There's fierce competition in the Massachusetts and certainly greater Boston market in healthcare between a number of systems. That has been wiped away. We virtually meet and talk, the leaders of the healthcare systems of Massachusetts, multiple times every day. We coordinate where to send patients, we move equipment around, we talk about what needs to be done multiple times a day. It's almost as if we have a single healthcare system at the moment in Massachusetts, which is again unprecedented. There's never been anything like it. That is really a bright point, I would say, and really gratifying to see,” Kevin said.
- Why we must temper our hope for a vaccine with patience and caution: “There is a lot of great work going on at our institution and around the country. We have somebody named Dr. Dan Baruch who's working with J&J on a potential vaccine, which is very promising, although there are lots of good groups around the country working on things. We're participating in many of the multi-center trials for a variety of different potential drugs,” he said. “I want to inject a note of caution, though. I think that there is a real obvious desire by everybody to find something quickly, but we need to be careful to study these things appropriately and not jump to conclusions. Unfortunately, there have been some examples, hydroxychloroquine being an example. But we don't know yet, and anecdotes are not only unhelpful, but also they can be harmful. We have to conduct these trials and do them well to see what helps and what doesn't, and we just don't know the answer yet. The fact that we all want an answer so quickly is understandable but that may lead us to the wrong conclusion. It’s highly unlikely that we are going to have a vaccine if we move at light speed in anything less than 12 to 18 months.”
Stephen Rosenthal on managing patient population health in a COVID-19 hotspot
In the sixth episode of the A Healthy Dose COVID Crisis miniseries, Trevor and Steve talk with Stephen Rosenthal, Senior Vice President of Population Health Management at Montefiore Health System.
Takeaways include:
- The origin story behind Montefiore’s Health System: “Montefiore has been around for quite a long time. It actually moved from Manhattan at the turn of the century up to the Bronx because back then the Bronx was basically just farmland and they were able to build a new facility there largely for managing patients with tuberculosis. So, Montefiore began with managing a pandemic of sorts. Actually one of our first buildings was the Florence Nightingale design because it was built as a T so that depending upon how the wind blew, the hospital would be able to create ventilation before there was air conditioning by opening the doors at either end of the corridors to create air flow in the buildings.”
- Insights into Montefiore’s patient population in the Bronx: “Of the 1.4 million residents of the Bronx, roughly 800,000 are Medicaid. So that's a substantial portion of the market of course, and that's probably the largest segment of our business model. Then there's a fairly significant Medicare population and they probably approach about 180,000 lives in the Bronx. But the interesting thing about that is that more than half of them are dually eligible. So you have a very poor and fragile population that depends on Medicare and Medicaid. The Bronx has a special need and clearly under this COVID experience the Bronx has suffered fairly significantly in the number of deaths from the virus.”
- How Montefiore quadrupled the number of ICU beds in two and a half weeks: “We’ve had the same operational team meeting every morning, seven days a week, dealing with summarizing all of the challenges within the healthcare system. One of the first things that we did, which actually is getting a lot of notoriety right now, is we created a critical care central command function. Now we had critical care beds in multiple locations around the system. As you pointed out, the need to get the right kind of service to an individual that needs to be intubated or managed with oxygen requires, supplies, whether it be oxygen or other related gases, and making sure that you can make those connections with the engineering staff and the related tools that are needed for that. You can't really imagine the complexity of managing from one location, all of those patients, but managing them in multiple locations would be undoable from a staffing perspective. So using digital technology in a centralized function, we were able to monitor all the patients in the various locations.”
Céline Gounder, M.D., on infectious diseases and COVID-19’s impact on public health

In the fifth episode of the COVID Crisis series, Trevor Price and Steve Kraus chat with Céline Gounder, an American medical doctor and medical journalist who specializes in infectious disease and global health. She was educated at Princeton University, Johns Hopkins Bloomberg School of Public Health, and University of Washington School of Medicine. She is also the host of two podcasts, American Diagnosis and EPIDEMIC Podcast.
In this conversation, Céline answers questions, such as:
- What actually is a virus? “A virus is an agent, a germ, that can hijack your host cells, your body cells, in order to replicate itself. It can't live on its own. A virus hijacks all of the enzymes and proteins, etc. that we use in our cells to replicate and the virus uses that machinery to replicate itself,” Céline explains. “Once it uses the cell, like a little manufacturing plant and produces its “big shipment, it bursts out of the cell and releases lots of new viruses, which then go on to create their next little manufacturing plant in another cell.”
- How potent is COVID-19? “This particular COVID-19 is not as deadly as SARS and MERS. (If a virus is much more deadly, then it sort of stops with that host much more quickly because they get sick and they're not able to pass it on.) But then you have diseases like the common cold that are caused by coronaviruses, which are far less deadly but very transmissible. COVID-19 is somewhere in between where it's very infectious, but it doesn't kill off every host it has, and we’ve learned that 25% don’t seem to have symptoms at all,” said Céline.
- How is this virus impacting the public disproportionately? “In terms of men versus women, we do know that there are some immunological differences between the two. Women are also at lower risk, at least until they go through menopause. Women are also at lower risk for cardiovascular disease, and we know that cardiovascular disease is actually a major risk factor for severe COVID disease. So there’s something immunologically as well as hormonally that's contributing to the gender differences,” Celine explained. “In terms of the race differences, we do not think that is a genetic issue. (We don't have any evidence for that right now.) We think that’s because of baseline health disparities, which we also saw in HIV, as well. For example, when HIV first emerged, it first hit the gay and trans population, and then spread out from there in concentrated populations that already faced health disparities. Some of that is from living in poorer neighborhoods, less access to education and quality healthcare. All of those things compound and leads to what we’re seeing. If you look at New York City data per capita, the highest mortality from COVID-19 is in the Bronx, and that is completely predictable, given social determinants,” she continued. “If you look at where the worst health disparities are and then if you look at the total number of cases, Queens has the highest total number of cases. Again, that makes sense if you look at the population distribution, who lives in Queens, and what kind of work that they have to do. Many people in Queens are working in service jobs where they don't have the luxury of telework for any number of reasons, right? So they are still having to go out there and are continually being exposed. It's not that people living in certain neighborhoods are innately more at risk for infection or disease, it's that they have to go out, and then they are exposed.”
Qventus’ Mudit Garg and Fairview Health Services’ Karyn Baum on preparing for patient surges

In the fourth episode of the COVID Crisis series, Steve Kraus and Trevor Price sit down with Mudit Garg, founder & CEO of Qventus, Inc, and Karyn Baum, VP of System Clinical Operations at Fairview Health Services. Together they talk about how healthcare systems are grappling with unprecedented patient surges during the COVID-19 pandemic. "Regardless of location, after seeing what's happened in New York, Italy, and beyond, hospitals can't afford to not be prepared to expand capacity and especially ventilator capacity," said Mudit Garg.
Top takeaways include:
- Why hospitals across the U.S. are experiencing drastically different capacity needs: “It's a tale of two cities across the country right now. Institutions, for example, in New York have field hospitals being served with thousands of beds, a majority of which are ICU and ventilator beds. That’s a massive undertaking,” said Mudit. “Think about if any business had to double or even increase their capacity by 25 to 30%? It’s not just about the physical asset of doing so. It requires nurses, respiratory technicians etc. However then there are other states have seen a major slow down because of social distancing, the cancellation of elective surgeries, and many of them are seeing record low levels of occupancy. It's the calm before the storm feeling for many places, such as Minnesota. But regardless of location, having seen what's happened in New York, having seen what's happened in Italy, and other places, you can't afford to not be prepared to expand capacity, and especially ventilator capacity.”
- The underreported story about the ventilator shortage: “The hospitals in New York are calling out for ventilators, but they are also calling out for really innovative solutions to get access to respiratory therapists,” noted Trevor. Karyn agreed and elaborated on his point: “Having a bed and a ventilator is necessary, but not sufficient. You also need somebody to run that ventilator, whether it's a nurse or a respiratory therapist or an intensivist. You also need people to draw labs. You need facilities management,” she said. “A hospital is a city of people and it's a huge amount of teamwork. It's the nurses and the respiratory therapists and those folks that are absolutely essential. During this time, healthcare systems have to think about how to have these people work in these environments, but also how to stay healthy in those environments.”
- A doctor’s perspectives on the emotional and physical toll COVID-19 is having on frontline workers: “We're proud of what we've done. We're sad at every patient we lose. Every patient you send home is a victory,” Karyn said. “We've had to have discussions with our family members we never thought we'd have to have, like, ‘Do I need to live separately from you for two weeks so that I don't bring this disease home to you?’ All of this reminds us of why we went to med school and why we love patient care.”
Ginger’s CEO on the effect COVID-19 is playing on mental health

In the third episode of the Covid Crisis series, Steve Kraus and Trevor Price sit down with Russell Glass, CEO of Ginger, to discuss the effect COVID-19 is playing on mental health and how the platform is stepping up to make sure our frontline healthcare workers have access to the mental health services they need. “If you’re looking at the active members on Ginger, we’ve seen a 50% increase from February to March,” said Russell. “We’re also measuring the intensity of these conversations from our care providers, and that is up by 10 to 15% during that same period. We’re just at the beginning, too, as we all move into this new reality.”
Top takeaways include:
- Ginger.io found that 70% of workers claimed that this was the most stressful time of their entire professional career, which includes periods such as 9/11 and the 2008 Recession. Based on a study Ginger did before and during COVID-19, they were able to see the real-time impact the pandemic has had on mental health. Russell told the podcast: “One of the stats we learned last year was that 48% of workers shared that they've cried at work due to anxiety and stress. This year that was up to 60% of workers. There's already an intensifying of what's going on in the workplace.”
- What inspired Ginger to provide their platform for free to all frontline health workers: "The vicarious trauma that this workforce is going through is going to be out of this world; it’s like nothing we’ve seen. It’s pre-trauma, too, so it’s anxiety leading up to knowing that you’re going to battle. It’s during; how do you manage your stress levels while you’re in the thick of it. And then it’s post, too, right? How do you make sure that you recover to go back the next day,” said Russell. “Because of this we launched three initiatives. The first is providing our coaching and content for free to all frontline health workers; the second initiative was just providing content out there that is relevant to the general public for free. Finally, we recognize that enterprises can't make long term decisions right now. They don't know what budgets are going to look like, so we’ve waived annual commitments. So, basically, a business can just get started with us and know that if you need to quit in two months, that's fine.”
- Why COVID-19 is a watershed moment for the future of telehealth and telemental health: “When you actually experience how convenient and just awesome an experience telehealth is compared to going into a doctor's office and all the downsides to that, you're a convert,” Russell said. “It's the kind of product experience that's high friction, but once you do it, you'll never go back. We learned from our research that about 38% of employees have tried some sort of telemental health or some sort of activity online for their mental health. Forty percent of those people tried it for the first time in the last four weeks.”
HealthReveal’s Lonny Reisman and Lori Bernstein on serving vulnerable populations most impacted by the pandemic

Lonny Reisman and Lori Bernstein are the founders of HealthReveal, a company that reduces healthcare costs while significantly improving quality of life for people with chronic disease. “We are in the business of trying to optimize chronic care management for health systems and patients,” explains Lori Bernstein. In the second episode of A Healthy Dose’s mini-series, the founders share what they’re seeing in terms of risk stratification as it relates to the Corona virus.
Takeaways from this conversation include:
- Insights into the most at-risk populations right now: “There are two major considerations: One, the socially vulnerable people who simply can't get by day to day without the resources have been developed and applied to support those people. The other characterization I would use is clinically vulnerable, people with chronic diseases, which until recently drove 80-90% of all medical costs and was responsible for a large degree of morbidity and mortality. Those clinically vulnerable people are vulnerable by virtue of their chronic diseases, but also that they're particularly susceptible to bad outcomes in the event that they're infected with COVID,” said Lonny. “If you couple a risk of, say, heart disease or diabetes or asthma or COPD with an infection, those, in fact, are the patients who are deluging the hospitals.”
- New pathways to serving patients outside of the ambulatory environment: “If you think about non-traditional pathways relative to tele-health, there could be a pop up dialysis center, for example, for the person that needs to get their dialysis or they're going to die, or there can be a remote stroke treatment program that one of our board members was mentioning,” said Lori. “These alternative workflows that HealthReveal can tee up based on our chronic condition report can help mobilize resources potentially that can come to bear that are outside the health system.”
- The flaws and opportunities this pandemic is exposing in the traditional brick-and-mortar delivery of healthcare: “What we're seeing is an underscoring of problems that have existed, at least certainly historically. I started my career working with patients with HIV,” said Lonny. “I was an intern in 1981. We saw, again, disparities in access, diagnosis, and I could list all the examples that have reared their ugly heads over the last 40 years. The silver lining is that hopefully we're learning, again, particularly as it relates to access to care for vulnerable populations, that there'll be a change going forward.”
Andy Slavitt on saving 40+ lives while we all #stayathome

Andy Slavitt is the former acting administrator for the Centers of Medicare and Medicare Services. “I made a promise to myself that after I left the [Obama] administration; I wanted to be a helper versus an insider,” he shared on A Healthy Dose. Today he’s a board member of the United States of Care and founder of Town Hall Ventures. In this COVID-19 mini-series on A Healthy Dose, Andy Slavitt shares a grounded perspective on how this pandemic will impact not just the healthcare system, but also the economy and society as a whole.
Critical insights include:
- Why shelter-in-place and quarantine are vital to prevent the exponential spread of the Coronavirus: “When you're chasing something exponential, something that's literally doubling every three days, it's like if you're 20 feet from a speedboat, and you swim 20 feet, and realize the speedboat is further away from you than when you started swimming,” explains Andy. “There was a month and a half that we lost based upon not getting proper tests. If we would have had testing and contact tracing in place, then people could socially isolate, quarantine, and prevent the outbreak, which is what we've done for other outbreaks. That was a function of the CDC telling the commercial labs not to produce tests. It was a function of the CDC not accepting the WHO test. The original sin may be tied to the President who had been tearing down every government bureaucrat in his mind. We saw a bunch of scientists that believed one way and the President was going out and saying the opposite...We've got to navigate from where we are, not from where we wish we were; we have to be focused less on the blame and a little bit more on how do we get ourselves out of this hole.”
- Insights from temperature data analysis and what that means for the projected spread of infection: “New Orleans right now is the hotspot of the world with 67% day-over-day growth. The Florida area, particularly the coastlines, is going to be bad. Detroit and Philadelphia are coming online next. We did some interesting analysis. We have access to real-time temperature data from people who take their temperature every day and they upload it to the cloud, and we're able to compare that to normal flu-like patterns,” said Andy. “We have been able to graph this against actions by governors and local officials to clamp down on social distancing, to enforce stricter and stricter rules on bars and restaurants, and we’re seeing that in those counties there are sharp declines in average temperatures. San Francisco, Santa Clara, had dramatic improvements early.”
- How you can save 41 lives by just staying home: “If you are an asymptomatic carrier and you infect just the average number of people, which is 2.3 people and that cycle goes on 10 times (e.g. each person infects 2.3 other people, and so forth) that’s infection 4,100 people,” said Andy. “If the case fatality rate is approximately 1%—Gates thinks it could be 1% to 3% and in Germany, it’s half a percent— as an asymptomatic carrier you’re responsible for 41 people losing their life.”
- Changes our country will have to practice as a result of this crisis: “With COVID-19, COVID-20, COVID-21, we are going to learn how to deal with infectious diseases in a way, hopefully, better than we ever have before. Getting public health money out of Congress has been virtually impossible,” said Andy. “In the future, we will hopefully do a much better job remedying this. It’s like you touch the hot stove. Our country needs to touch every stove once, but then we get really good about being inventive, and creative, and solving these things. On an ongoing basis, we're going to have as deadly diseases come and go, whether they're seasonal or otherwise and are part of our lives. We'll have vaccinations that sometimes work better than others. This will be a strain much like the flu, except deadlier and more infectious. And, during those periods of time, we're really going to want to watch out for the vulnerable people in society.”
- Parting thoughts on how to help stop the spread: “If you approach this with the spirit of I'm [staying home] with a purpose, I'm saving 40 lives, I'm making a sacrifice for my country, it's not forever. We're going to get through this, the only question is when we get through this, how many casualties will there have been?” shared Andy. “All of us are going to look back on this era of time and ask ourselves, ‘What were we doing?’ We all want to be really proud of what we did. So if that means bringing soup over to an elderly neighbor's house or talking to her through her door or FaceTiming people to check-in, etc. that makes an impact... History has shown that those periods of time when people are uncertain and people are scared, a lot of amazing things happen too during that time. A lot of sad things happen, but a lot of amazing things can happen too.”
Listen to all these insights and so many more in this episode of A Healthy Dose.
Q: What are the opportunities for founders given the COVID crisis?
Jeremy Levine, partner at Bessemer Venture Partners, shared his thoughts on a new landscape reshaped by the coronavirus and for CoderPad’s just-launched Good Perspective series. Read the full article here.
Top takeaways:
- Entrepreneurs should focus on survival: “2020 will be the lost year for many companies,” said Levine. “It matters less what happens this year as long as you survive with sufficient resources to compete in 2021. Take the necessary actions now so you have what you need to go on the attack when this passes.”
- Founders have a talent opportunity: “For founders, this is an opportunity to pick up people you had no chance of landing six months ago when the labor market was much tighter,” Levine said. “If your company has the chance to do that, you should think seriously about it.”
- While the landscape is divided, some sectors are experiencing tailwinds: “People are spending their time at home with more limited entertainment options so video game and remote learning companies are actually doing great,” observed Levine. “Think sites like Discord or services like Teachable. They’re now confronting all the good problems to have: taking advantage of an unexpected influx of new users, deciding how to manage a fresh cash infusion, and building deeper engagement with their existing user base.”
Q: How should I think about cash management and fundraising in an economic downturn?
Partner Byron Deeter and SaaStr's Jason M. Lemkin went live to discuss the state of venture capital and the cloud industry, given the economic downturn. Together, they answer what founders should do when raising venture dollars and how to manage their cash runway during a bear market.
Top insights from their conversation include:
- "The easiest VC discussions to engage in right now are the ones where there is a pre-existing relationship," said Byron. If you're building a net new conversation right now with a new firm or investor, don't take offense if you don't hear back from them right away. Most firms are doing work internally and helping triage their portfolio. A month from now, follow back up.
- If you have financing discussions and momentum underway, try to close them out as soon as possible. Don't try to over-optimize price, valuation, and terms at this time. "Think speed over greed," said Byron. However, if you haven't started your fundraising efforts just yet, hit pause, and wait a few weeks for the dust to settle. It's always difficult to close a deal with people you've never met before in person, so expect that the process might look different and take more time considering the current circumstances.
- Almost all companies are going through scenario planning, hiring freezes, and setting up new dashboards and forecasting metrics. If you are a venture-backed business with 18-24 months of runway, take advantage of the next two quarters. Byron and Jason recommend doing all, or a combination, of the following: 1) develop your management team, 2) assess where your product is falling short and evaluate your feature gap list, and 3) reflect on what you can do to become a more resilient business in 2020.
- "The magnitude and the speed of this pullback across all sectors is unprecedented. This is the fastest 30% decline in the market in history and it beats The Great Depression, the dot com crash, and The 2008 Recession," said Byron. "The silver lining is that there will be a finite end to this recession, though, it's dependent on the mass production of vaccines, which experts say won't be available for 9 to 18 months. While there could be an economic lag that's dependent on a vaccine, we can expect to see a rebound cycle after that."
- "At Bessemer, we've seen fantastic companies get their start during the last recession, including Twilio, Shopify, Pinterest. We are very cognizant that great entrepreneurship happens across all cycles–and while the exits tend to cluster, the entrances don't," said Byron.
Q: How should I value my startup during a downturn?
With the economic downturn in the public markets, private market valuations are also being impacted. Mary D’Onofrio explained this nuanced dynamic recently with TechCrunch. As one of the authors of 10 laws of cloud who also helps run the Bessemer Emerging Cloud Index (^EMCLOUD), Mary understands the links between private valuations and public share prices. Read the full article here.
Top takeaways on her perspective:
- “What’s important to know is that outside of a market disruption, cloud software tends to trade on revenue and revenue growth. Companies should fundamentally be valued on the present value of their future free cash flows. But I think with cloud software, in particular, there’s a prioritization of taking [market]share, and then applying a very long term healthy margin structure on a very massive revenue base once you get there, and generating cash then.”
- “The way that I like to think about valuing companies is what can it become in the future, and then discount that back to today insofar as private market valuations are concerned.”
- “[We] evaluate on forward growth because you’re looking at the future free cash flows; you’re not looking at what it is today, you’re looking at what it can be in the future, and if you’re looking to value the future, you need to in fact look at the future.”
- “Investors need to find a valuation that makes sense for your model, what the market expects, and what the founder will accept,” writes TechCrunch. Mary adds another: “The forth criteria is making sure that the valuation still meets your cost of capital and your returns thresholds. And so to some extent there’s a little bit of a valuation game as well where — I wouldn’t call it disconnected from fundamental value — but there’s a certain extent to which your maximum price that you might be willing to pay today is really what do I think it can become throughout my hold period, apply my multiple there at exit, and then discount back to today by my cost of capital or by my cash return needs. And that would be your ‘max valuation.’”
Q: How can I manage churn and customer retention rates?
You can get all the slides to this presentation here.
In this conversation with Gainsight, Byron Deeter shares the multi-scenario perspectives leaders are having at the board level, insights into the volatility of the market and private valuations, and the four major categories (geography, industry vertical, functional vertical, and customer segmentation) that cloud founders can use to understand their exposure to the current market environment.
As SaaS leaders tackle the unexpected management implications of COVID-19, there has never been a better time to double down on retention strategies to minimize churn.
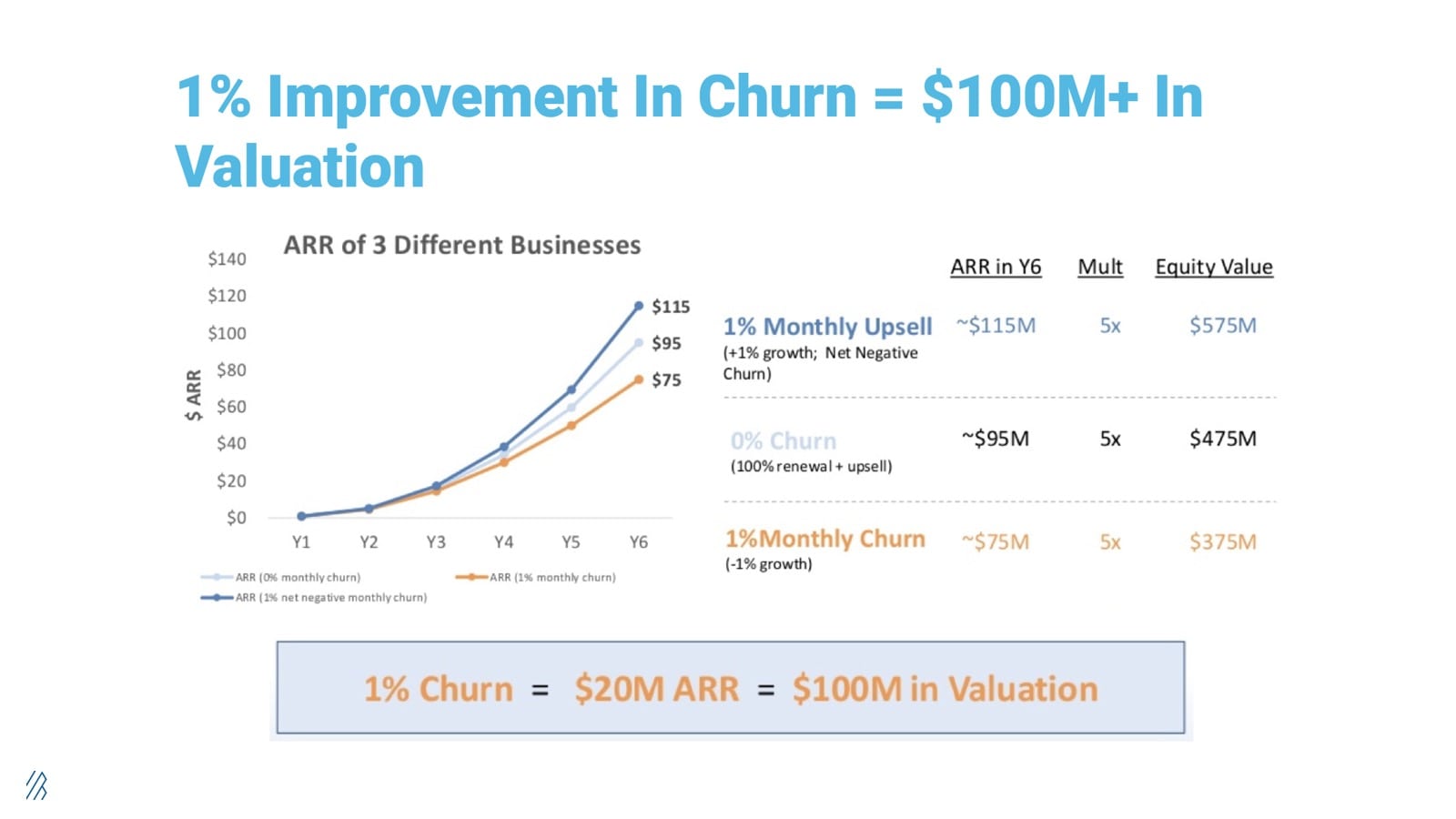
“One percent improvement in churn can equal $100 million+ in valuation by virtue of the free cash flow it creates,” said Byron.
The most profitable business any company can have is the recurring revenue of its customers. Keeping those customers during this time is the lifeblood of your business. The recurring revenue will be what allows your company to maintain headcount, have stability, and [customer success] can be the rock to get you through this time.”
Watch the full video and get all the slides here to learn the strategic and tactical steps from Gainsight on how to minimize churn during a downturn and prepare a playbook to negotiate at-risk customers.
Q: What are the metrics that matter most right now for enterprise software companies?
Elliott Robinson offers insights to Brian Hollins on The Road Untraveled about how venture-backed startups can get the most from their VC partners during these times of uncertainty. In this conversation, Elliott shares that experienced functional experts are a wealth of valuable insight, and then he dives into the operating metrics that enterprise software companies need to keep a close eye on, more than ever before.
Key Takeaways:
- Tap into the platform and community resources to learn from the experts and operating leaders that can provide counsel for long and short term steps. It is critical to “dial in” to the leaders around founders to help them fill in the gaps of their expertise
- “One of my portfolio companies has completely changed its messaging on its website, email, and digital marketing for the crisis,” said Elliott. “In the world where your value proposition is expansive, you might want to narrow it down so your messaging is contained into what matters most to people given this current crisis. That was something one of our executives-in-residence guided our team on the other day.”
- Firms and companies alike will need to get prepared to hire individuals who they may have never met in person. There are lots of ways to still do effective diligence and make good decisions.
- “Gross margin payback period is still my number one unit economic indicator of success. Based on your business model and delivery model COGs how many months does it take to get a customer profitable? In a world where churn will most likely increase across all sectors that’s even more important,” Elliott explains. “Because if your CAC is really high and it takes you 22 months to turn a customer profitable, on a gross margin basis, then the next 22 months could be a wasteland. Let’s say we make it six months out of this downturn, and you bring on more customers, then you have to wait another 22 months to turn them profitable. Businesses in that 6-12 month cac payback range are in a better position right now, especially if they're able to cut costs, and keep churn relatively okay. When we do enter a recovery, they’ll start seeing operating leverage in their business faster than others.”
Q: What are the best practices to transition to work from home (WFH) in a hurry?
Wade Foster, CEO and co-founder of Zapier, a Bessemer portfolio company, hosted a virtual AMA panel on remote work featuring Michael Pryor, co-founder of Trello, Natalie Nagele, co-founder of WildBit, Kieran Flannagan, VP of Marketing at HubSpot, and Sarah Park, president at MeetEdgar. Here were the top insights and takeaways from this conversation.
Redefine WFH productivity:
Schedules are disrupted, daycares and schools are closed, people are possibly recovering from being sick or even struggling with anxiety. When it comes to redefining productivity in a new work from home setting, here are seven suggestions and productivity tips.
- Sit down with your partner or house/roommates and set a game plan on how to make this new set up work. Clearly communicate goals and priorities so everyone not only has a quiet place to focus and take calls but also shared responsibilities are still addressed.
- As a co-worker, be empathetic and understanding if your colleagues have to unexpectedly reschedule and/or tend to childcare.
- Considering the cognitive load COVID-19 is adding to people’s psyche and strive to be a supportive co-worker. Some people cope by diving into a work project, whereas others might need more space to stay focused and follow through on deliverables.
Adapt to a new WFH routine with these habits:
- Kieran: “I always plan out my day the night before. I stack rank my priorities and put them in my calendar. I also have the same playlist I listen to every day that helps me stay focused.”
- Sarah: “I create ‘sun breaks’ in the day where I go outside. I also end my day with a ‘commute’ by scheduling a walk so that I leave my home office and separate my work life with my home life.”
- Natalie: “Cal Newport’s Deep Work reminds us that it’s our personal responsibility to understand what makes us most productive. As a manager, my schedule can get loaded with meetings so I block out quiet time so I accomplish my top priorities.”
- Michael: “When your wheels are spinning, it’s important to just get your ideas out of your head and write them down so you can focus on what needs to be done. At Trello, we also rely on the DACI framework. When having to make a group decision, clearly define who is the driver of the project, who is the approver, who is the contributor, and who needs to be informed of the final decision.”
Practice good management while remote
- Lead with trust and don’t start getting hands-on until the deliverables are not meeting expectations. It’s easy for managers to become micromanagers during the WFH transition, and it’s not necessarily about having daily standups, either. The fastest way to build trust in this new work setting is to communicate very clear goals and shorten the delivery cycle. By creating smaller accomplishments, people feel the momentum of working together remotely. Over time, these delivery cycles can be stretched out as teams tackle larger projects.
- Practice your communication skills through remote meetings. “Remote work is more or less difficult depending on the personalities,” says Kieran. “I’ve learned that it requires people to practice storytelling and getting better at presentation skills.”
- With video conferencing, all team members should stay eye-to-eye. “Even if the office has a camera for the room, I always call in from my laptop so that my face is in the virtual grid with everyone else. It’s a small habit that puts everyone on the same playing field,” says Michael.
- If there seems to be a miscommunication via Slack, always escalate to Zoom. In chat, people miss the nonverbal cues. If the miscommunication happened in a public group, follow back up with the team and let everyone know the conclusion.
- Use check-ins to celebrate progress and also provide feedback and course-correct along the way. As Andy Grove suggests in his book High Output Management, a high-performer might need more frequent check-ins and milestones as they take on a new type of project that’s outside their wheelhouse.
- For team members: As tasks are accomplished and progress is made, leave evidence that you’re following through on your promises through status updates via Slack, shared docs, and emails, etc. Priority trackers not only help team members demonstrate to their remote manager that they’re driving value, but they also give a team member a moment to reflect throughout the week and determine where they’ve succeeded or where they’ve gone off track.
Build a community to stave off loneliness
Productivity levels are highest at companies when people are engaged at work and feel like they’re part of a community. Here are five tips on how to build a virtual team with a strong sense of belonging:
- Sarah: “Similar to how you might strike up a conversation in the office, you can create spontaneity, remotely, by prompting water cooler conversations. We have a Slack channel that’s dedicated to a question of the day to give people a way to engage with their co-workers when they need a break. We’ve also tried different activities like streaming a movie so everyone can watch it at the same time. Building fun and engaging community remotely is about getting creative with what you do normally in an office but recreating it virtually.”
- Natalie: “It’s about moments of intention. Not all companies are logged into Slack all day. Every Monday morning we have an automated question: “How was your weekend? What did you do?” People share their stories and photos from the weekend. On Fridays we do Demo Days where someone does a show and tell; for example, someone once shared their wine selection. It’s a way for us to get to know people on a more personal basis.”
- Michael: “Once a month, we do virtual Town Halls where everyone is logged onto Zoom. And then we do what we call “Mr. Rogers” where team members are grouped into 4-5 people so that people can have 15-20 minute conversations through Zoom. It's a great way for people across the organization to meet one another and also have personal conversations.”
- Wade: “Once a support engineer at Zapier suggested we have a dance party. They selected the song on Spotify and then told everyone to dance and create a gif through GIPHY. Then, everyone uploaded it to Slack!”
- Kieran: “All of the remote life is on scheduled time, so as a manager it’s important to facilitate that connection and conversation every time you are face to face with your team. Spend the first five minutes of each meeting talking about that person’s life or catching up on what’s new for them. It goes a long way.”
Q: What are the ways that I can contribute to the cause?
#StopTheSpread
Guild Education's CEO Rachel R. Carlson and Kenneth Chenault launched StoptheSpread.org, a grassroots movement to lead the private sector’s response to COVID-19. #StopTheSpread asks its 1,500 signatories to help fund healthcare needs and do one of the following:
- Pay it forward: #StopTheSpread asks large companies with flexible balance sheets to immediately pay their small business vendors rather than waiting 30-45 days to pay their accounts payable.
- Support the frontline workers: #StoptheSpread is launching an effort with a number of universities around the US to offer COVID-19 training programs so workers in healthcare, retail, manufacturing, etc. learn how best to protect themselves and navigate conversations with their managers if they still have to go into work.
- Serve your hometown: We ask that celebrities and business leaders follow Steph Curry and Ayesha Curry and support their local community. The Currys are supporting kids who no longer can rely on school lunch with the funding for the Alameda County Food Bank through the crisis.
Our gratitude goes out to the people working at the frontlines in healthcare, public service, groceries, and more. As we shelter in place, corporate leaders, such as Twilio, PagerDuty, Zoom, Toast, Zapier, and many more, have already took the pledge to #StopTheSpread.
MoneyDuringCorona.com
MoneyDuringCorona.com helps hourly workers who were recently laid off find temporary jobs across 15 metro regions in the United States. Unlike other job boards, the site is built specifically in mind for those impacted by the corona crisis, featuring real-time text updates and new job opportunities.
Bonus: What good news can I read?
In trying times it’s natural to fixate on the negative news streaming on our feed. However, this is no time to ignore all the helpers out there doing their part. Here’s a recommended reading list about the leaders and organizations supporting the workers at the frontlines in healthcare, small businesses, manufacturing, including teachers, parents, and more.
Recommended reading list:
Ken Chenault and Guild Education’s Rachel Carlson
Zoom: CEO Eric Yuan is giving K-12 schools his video conferencing tools for free
Toast: Support restaurants with the #RallyforRestaurants challenge
Twilio: How Twilio.org is supporting COVID-19 crisis response efforts
PagerDuty’s Jenn Tejada takes the pledge to #StopTheSpread
Zapier: A note from Zapier’s CEO to COVID-19 responders
Stephen and Ayesha Curry: How they are supporting Alameda County kids and families
Nick Mehta and Gainsight HQ are proud to be a part of #StopTheSpread
How Christian Siriano turned his fashion house into a mask factory